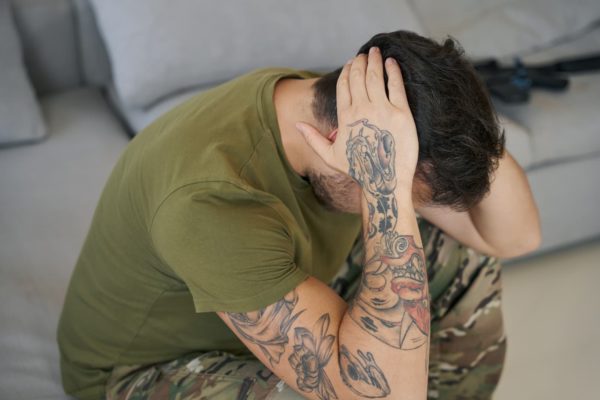
PTSD Meaning: What is PTSD?
PTSD stands for post-traumatic stress disorder. Whilst the term was first coined in the late 1970s the first descriptions of what is now known as PTSD were described many years prior. In 1952, the term “great stress reaction” was included in the first classification system of mental health conditions and bears similarities to the current definition of PTSD.
The well-known term ‘Shell shock’ was given to those in the military who suffered PTSD, however it is a common misconception that PTSD only affects those affected by war. PTSD has also been shown to be highly prevalent in the civilian population.
PTSD is a form of anxiety disorder. Sufferers often experience nightmares and flashbacks of the traumatic event that triggered their PTSD, they may also experience feelings of guilt, irritability, and isolation. Amongst other side-effects, PTSD can cause insomnia and difficulty concentrating, making daily life difficult.
What Causes PTSD?
There is no one cause for PTSD, however it is typically due to exposure to traumatic events “outside the range of normal human experience”. However, not every individual who is exposed to a traumatic event will develop PTSD
There are an unknown number of events which may lead to the development of PTSD. These include but are not limited to:
- Being involved in a car crash
- Experiencing violence such as military combat, acts of terror, domestic abuse or other physical assault
- Experiencing abuse, whether sexual, bullying, harassment (including racism, sexism, homophobia, transphobia or biphobia or other identity-based abuse)
- Being raped or sexually assaulted
- Death of a loved one
- Witnessing something traumatic
- Work-based trauma such as that experienced by those in the emergency services and military
- Diagnosis of a life-threatening/altering condition
People with other mental health conditions or with limited social support groups may be at an increased likelihood of developing PTSD compared to others.
PTSD Symptoms

The most typical symptom of PTSD is re-living or re-experiencing the traumatic event in the form of flashbacks and/or nightmares. Other symptoms of PTSD include but are not necessarily limited to:
- Repetitive visions or sensations of the event and physical sensations such as pain, sweating, nausea or shaking
- Night terrors and difficulty sleeping
- Avoidance. The sufferer may avoid certain locations or people that act as reminders of the event and may not speak of the event to push it to the back of their mind. Avoiding reminders of the event is sometimes used as a coping mechanism though it is not considered a healthy way to manage PTSD.
- Feeling ‘on edge’. A person living with PTSD may feel very anxious and ‘jumpy’. They are constantly aware of potential threat (even where the is none) and are easily startled. The clinical term for this is ‘hyperarousal’ and it can lead to irritability, anger and angry outbursts, poor sleep, and difficulty concentrating
Complex PTSD
Contrary to some information, there are not multiple types of PTSD. However, complex PTSD has additional symptoms to the regular signs of PTSD which include:
- A lack of control over one’s emotions
- >Feelings of anger or distrust towards the world and those in it
- Persistently feeling empty or hopeless
- Believing oneself to be damaged or worthless
- A loss of friendships or relationships through avoidance
- Feeling disconnected from oneself and the world around them (dissociative symptoms)
- Physical symptoms such as headaches, dizziness, chest pains, and stomach aches
- Sufferers may feel as if they are completely different to other people and like nobody can understand them;
- Some may also experience feelings related to suicide or self-harm
PTSD Diagnosis
Following a traumatic event, it is normal to feel upset or confused, and it may be appropriate to seek help to process the acute thoughts and emotions one may experience as part of a normal or acute stress response. However, if symptoms persist for 4 weeks or more this may represent the development of PTSD and may benefit from seeing an appropriately trained healthcare professional. There is no specific PTSD test, diagnosis is given following a full assessment by a GP and/or mental health specialist.
Typically, an initial assessment is done by a GP. If they have appropriate training and experience, they may be able to make a diagnosis. However, in most cases referral to a mental health specialist with expertise in PTSD is required.
In the UK, a referral to a community mental health team through the NHS can then be arranged. Private healthcare is also an option.
PTSD Treatment: How is PTSD Treated?
PTSD can be treated years after the event – it is never too late to deal with the traumatic event.
Prior to forming a treatment plan, a comprehensive assessment of symptoms will be completed by a healthcare professional. The main treatments for PTSD are talking therapy and medication.
Specific talk therapies which focus on trauma are available for those with PTSD, such as trauma-focused cognitive behavioural therapy (CBT) and eye movement desensitisation and reprocessing (EMDR).
Medications, typically take the form of antidepressants, such as venlafaxine and selective serotonin reuptake inhibitors (SSRIs).
If symptoms have not persisted for more than 4 weeks, a period of active monitoring may be recommended – this is where the affected person monitors their symptoms to see whether they improve over time. A follow up appointment will normally be scheduled within one month.
PTSD and Medicinal Cannabis

Research into the effect of medicinal cannabis on PTSD is limited. However, following the legalisation of cannabis for medical purposes in 2018, there has been a rise in people looking towards medical cannabis. When first-line therapies have not proved effective at reducing symptoms, medical cannabis may be considered an option for PTSD.
For further information and to find out more about medical cannabis, click here to discover more about our award-winning Curaleaf Access Scheme. Alternatively, complete an eligibility assessment now. Once complete, one of our clinicians will review your application and advise whether you are eligible for progression to an appointment.

